Some Known Details About Medigap Cost Comparison Chart
Wiki Article
What Does Medicare Part G Mean?
Table of ContentsThe Definitive Guide to Shingles Vaccine CostMedicare Part G for DummiesThe 8-Minute Rule for Medigap Cost Comparison ChartThe Greatest Guide To Medigap Cost Comparison Chart


Usage Method B for revenue as well as assets. Keep in mind: If people that are also qualified for MA meet greater than one basis of qualification, they may pick the most useful basis for MA, however should utilize a Method B basis for the Medicare Financial Savings Program. Possession Standards Possession restriction is: l $10,000 for a family of one.
Instance: Bud's earnings is 125% FPG. He is ineligible for QMB also if he has covered expenditures that would permit him to spend to 100% FPG. Covered Services (Prepaid MHCP Handbook) The advantages of the QMB program are: l Payment of Medicare Component An and Component B costs. l Payment of Medicare cost-sharing (co-payments as well as deductibles) for Medicare solutions provided by Medicare-eligible carriers.
It is hardly ever helpful for individuals in LTC to be QMB-only due to the fact that: l Medicare Part A covers extremely restricted competent nursing care. l Payment might not be confirmed up until a number of months after the treatment is gotten. Nonetheless, if you recognize Medicare Component A is covering any of the LTCF expenses, it is advantageous for individuals to be QMB-only because there wouldn't be an LTC spenddown.
The Buzz on Medicare Supplement Plans Comparison Chart 2021 Pdf
People might receive MA and QMB simultaneously. l People with revenues at or under 100% FPG receive QMB, as well as likewise for MA without a spenddown if their properties are within MA limits. l Because QMB enables a basic $20 income neglect and MA does not, people with earnings over 100% FPG yet no even more than 100% FPG + $20 are within the QMB revenue restriction however must satisfy a spenddown to get approved for MA.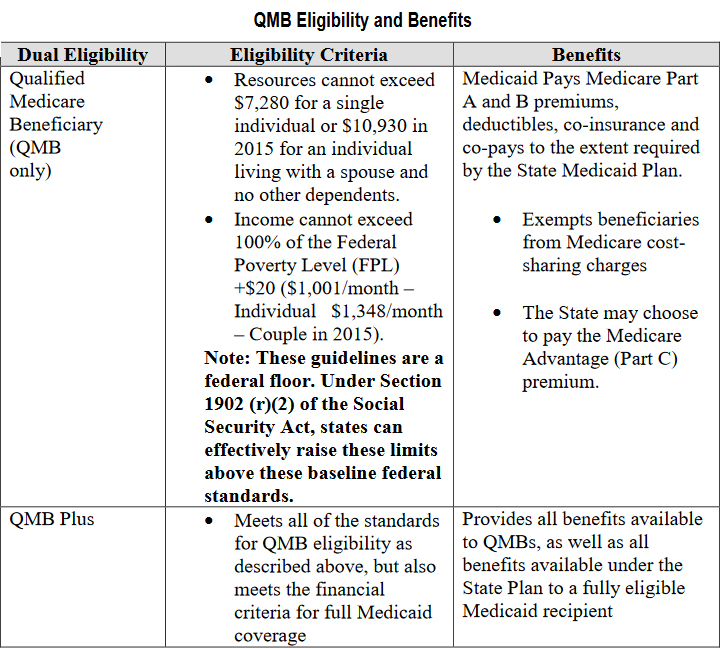
Activity: Due to the fact that Blanche's possessions are within the QMB restriction but not the MA limit, approve her for QMB only.
Medicare Savings Programs (MSP) assist individuals with limited revenue and resources pay for some or every one of their Medicare costs and may additionally pay their Medicare deductibles and also co-insurance. There are four different types of Medicare Cost savings Programs, this web page focuses on the Qualified Medicare Recipient (QMB) Program. Who Certifies? If you have earnings from functioning, you may get advantages also if your earnings is more than the limitations listed.
Aarp Plan G Things To Know Before You Buy
See the Benefits and also Solutions Review for a listing of Health and wellness First Colorado co-pays. How To Apply Where Do I Obtain These Services? You can visit any type of doctor that accepts both Medicare and also Health and wellness First Colorado coverage. See our Discover a Doctor web page to look for Wellness First Colorado providers.You can additionally visit the Medicare website to look for Medicare companies. If you have more concerns about this program please see our Medicare/Medicaid Frequently Asked Questions or contact our Member Get try this web-site In Touch With Center. Program Contact: , 303-866-5402. The participant's advantages are limited to payment of the participant's Medicare Component B premium only. Service providers ought to tell the participant that the service is not a Medicaid-covered service for a participant that has just SLMB coverage. When the EVS recognizes a participant as having actually just Specified Low Earnings Medicare Recipient insurance coverage (without additionally having Complete Medicaid or Package A protection), the supplier must call Medicare to confirm clinical insurance coverage.
When the EVS determines a member as having Specified Reduced Revenue Medicare Recipient protection as well as also Complete Medicaid or Bundle A coverage (without waiver liability), Medicaid asserts for solutions not covered by Medicare needs to be submitted as routine Medicaid cases and not as crossover insurance claims. The member's benefit is payment of the participant's Medicare Part B costs.
The member's advantage is settlement of the participant's Medicare Part A costs. The EVS identifies this protection as Professional Medicare Beneficiary - medicare plan f.
Medigap Cost Comparison Chart - Truths
Yearly modifications in the FPL indicate that, also if you may not have actually gotten QMB last year, under the brand-new FPL, you might be able to certify this year. To get the QMB program, you will certainly require to contact your regional state Medicaid office. For more support, you might desire to call your neighborhood State Medical insurance Assistance Program (SHIP) - medicare select plans.
SPAPs are state-funded programs that supply low-income and medically clingy elderly people and people with impairments economic aid for prescription medicines. aarp g. We have SPAP info online right here (note that the SPAP info is subject to change without notice): If you do not fulfill the low-income economic demands to get approved for the QMB program, you still may have some of your Medicare prices covered by one of the other Medicare Cost Savings Programs.
The FO takes the application as well as processes it according to instructions in HI 00801. 140E.4 of this area. Example of individual asking for Premium-Part An as well as Part B enrollment throughout an enrollment duration: Ms. Adler resides in Pennsylvania (a Component A Buy-In State) as well as does not have Medicare. She contacts her regional FO in January 2018 since she wants Medicare coverage however can not pay for the premiums.
Adler may submit an application for "conditional enrollment" in Premium-Part A. Because Ms. Adler lives in a Component A Buy-in State, the Component B and conditional Part A registration can be filed any time. The application is not processed as a General Registration Period (GEP) application. The FO takes the application as well as refines it according to instructions in HI 00801.
Report this wiki page